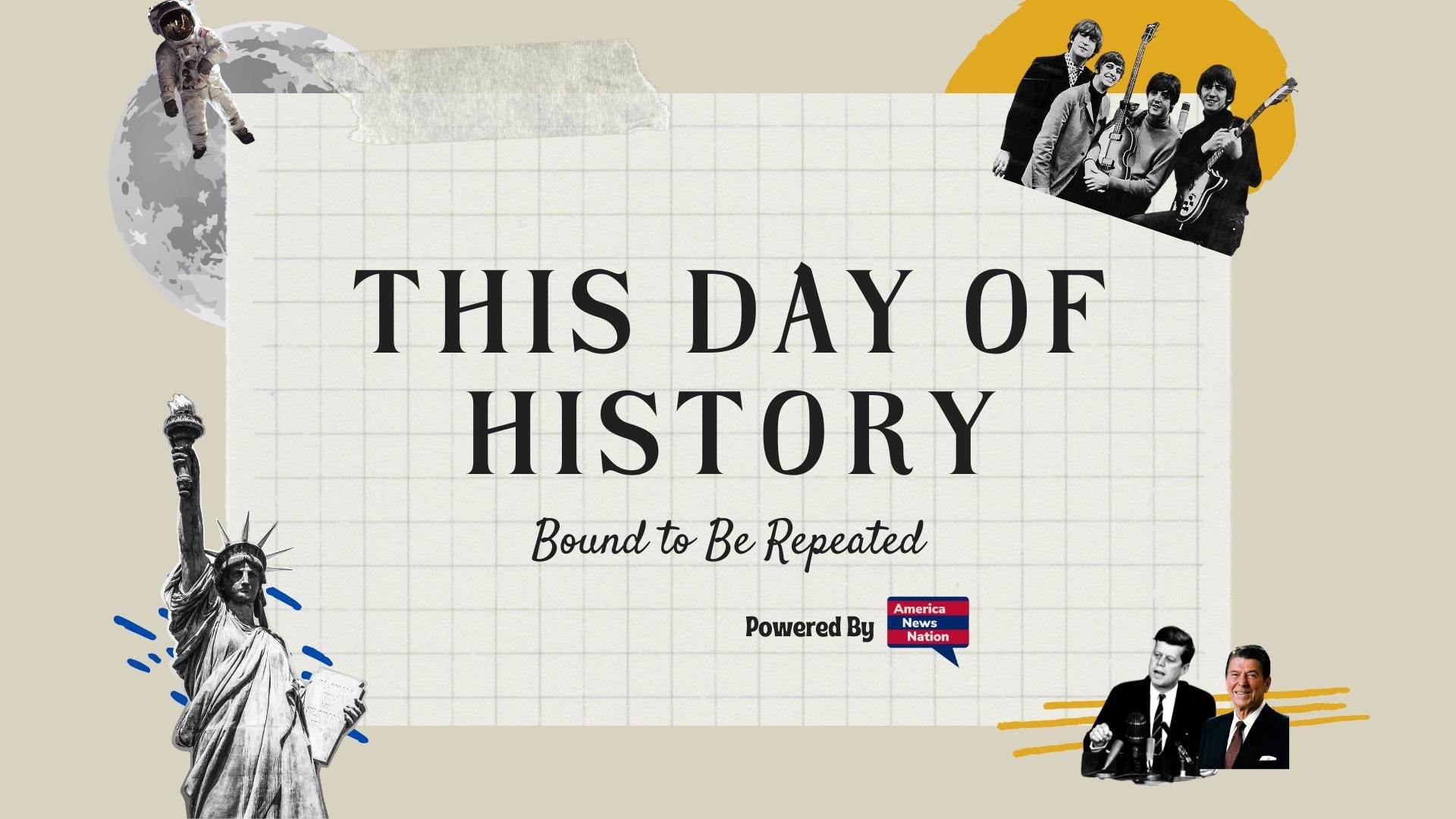
On October 19, 1943, in a modest laboratory at Rutgers University in New Brunswick, New Jersey, a quiet scientific revolution took place. A research team led by microbiologist Selman Waksman and his graduate student Albert Schatz successfully isolated streptomycin, the first antibiotic effective against tuberculosis (TB)—a disease that, for centuries, had been among humanity’s deadliest scourges. The discovery transformed modern medicine, turning a once near-certain death sentence into a curable infection and launching a new era in antimicrobial therapy.
The path to streptomycin began with Waksman’s fascination with soil-dwelling microorganisms. He theorized that some microbes in the earth produced natural substances capable of inhibiting the growth of harmful bacteria—a concept that would become the basis of the field he named antibiotics. In the early 1940s, his lab systematically screened thousands of soil samples for bacteria-fighting compounds. Schatz, a 23-year-old graduate student working under Waksman, focused on organisms known as actinomycetes—filamentous bacteria common in soil.
In October 1943, Schatz isolated a strain of Streptomyces griseus from a soil sample collected on the Rutgers campus. From it, he extracted a substance that inhibited the growth of Mycobacterium tuberculosis—the bacterium that causes TB. Waksman named the compound streptomycin, following his convention of naming antibiotics derived from Streptomyces species. Initial tests on laboratory animals showed remarkable success: streptomycin not only suppressed the TB bacteria but did so without the severe toxicity that plagued earlier experimental drugs.
The impact of this breakthrough was immediate and global. Tuberculosis had ravaged populations for millennia, killing one in seven people in the 19th century and earning grim nicknames such as the “white plague.” It struck indiscriminately—young and old, rich and poor—and filled sanatoriums around the world with patients consigned to isolation and slow decline. Before streptomycin, treatment consisted mainly of rest, sunlight, and fresh air—ineffectual comforts against a bacterial disease that had no true cure.
When clinical trials began in 1944 under the U.S. Army’s guidance, the results confirmed streptomycin’s potential. The first patient, a 21-year-old woman named Patricia “Patsy” T., was dying of advanced tuberculosis meningitis. Within weeks of receiving streptomycin, her symptoms improved dramatically. Although she eventually relapsed—later understood to be due to bacterial resistance—the case proved that antibiotics could defeat TB, at least temporarily. Soon, pharmaceutical companies such as Merck and Eli Lilly scaled up production, supplying the drug to military hospitals and civilian clinics worldwide.
Streptomycin’s discovery also reshaped the field of microbiology. It was the first antibiotic found to be effective against gram-negative bacteria—a group that includes pathogens responsible for diseases such as typhoid and plague. Its success prompted an explosion of research into soil microbes, leading to the discovery of dozens of other antibiotics, including tetracycline, chloramphenicol, and erythromycin.
Yet the triumph was shadowed by controversy. A bitter dispute erupted between Waksman and Schatz over credit for the discovery. Waksman, a seasoned researcher and public figure, initially received sole recognition, culminating in the 1952 Nobel Prize in Physiology or Medicine “for his discovery of streptomycin.” Schatz, feeling overlooked, sued Rutgers and Waksman, arguing that he had performed the crucial isolation work. The case was settled in 1950, granting Schatz legal recognition as co-discoverer and a share of royalties—a rare acknowledgment for a graduate student at the time.
Despite the controversy, streptomycin’s legacy remains monumental. Its introduction marked the beginning of the end for tuberculosis as a dominant killer in industrialized nations. Combined therapies—streptomycin with drugs like isoniazid and para-aminosalicylic acid—soon became the global standard, cutting TB mortality rates by more than 90 percent in the ensuing decades.
The ripple effects extended far beyond medicine. Streptomycin demonstrated the power of university-based research, bolstering support for federal science funding in the postwar era. It also showed how collaboration between academia and industry could yield lifesaving results.
Today, even as multidrug-resistant TB strains threaten a resurgence, the story of streptomycin endures as a cornerstone of biomedical history—a testament to curiosity, perseverance, and the life-giving potential hidden in something as ordinary as a handful of soil.